This article has been written especially for Helping Hands and comes from Brendan McCormack work at Queen Margaret University, Edinburgh along with other practices.
About Brendan McCormack

An Introduction To Person Centred Practices
As I write this article, we are in the middle of the Global Coronavirus (Covid-19) pandemic and all of us are adjusting to new ways of living our lives, creating new social norms and developing new perspectives on resilience and personal strengths. It is fair to say that none of us could ever have anticipated this scenario when we celebrated the arrival of 2020 and the ‘year of the nurse and midwife’. The focus that will be placed on nursing this year will be momentous and a landmark in nursing history in terms of the contribution that we will make to the lives of populations at this time. Of course, nurses don’t work in a vacuum and that is especially the case in community care/services, where the work of nurses happens alongside and along with a cadre of social care workers who provide day to day support to thousands of older people and people living with long-term conditions in communities across the UK. This challenging period we are living in also focuses our minds on ‘who we are as persons’ which is the foundation focus of person-centred practice, given that so many aspects of our lives are being called into question, readjusted, realigned and fundamentally changed – temporarily or permanently! So, it is a good time to explore person-centredness and person-centred practice.
Discovering Person-centredness
Since starting out in my nursing career at the age of 18, I cannot remember a time when the needs of persons were not my top priority. However, it is only in the past 20 years or so that it has truly become a vision for healthcare and one that has been a life-long ambition for me achieving as a global philosophy – and of course like all good visions, will outlive me completely!
Person-centred practice has been in the literature in various shapes and guises for many decades, but the ideas written about were not conceptualised in that way. As a student nurse, I was introduced to nursing theories and studied many of the nursing models and frameworks of the great ‘giants’ of (mostly American) nursing theory (such as Virginia Henderson 1966; Imogene King 1971; Dorothea Orem 1991, to name but a few!). These theorists expounded the meta-theory of nursing (Lee & Fawcett 2013) and articulated the interrelationship between person, environment, health and nursing. Depending on their philosophical perspective, the relationship between these four constructs created a different approach to how persons were perceived and thus how we as nurses operationalised our role. I remember being fascinated by the work of Dorothea Orem and studied her theory of nursing and implemented it in practice.
Issues such as these dominated my thinking about my practice for much of my early career in nursing. While debates about nursing theories, the role of the nurse, the science of nursing practice and the search for an evidence-base persisted, it became abundantly clear to me that day-to-day experience of patients and staff wasn’t changing significantly and we as nurses continued to practice in the same ritualistic and routine ways regardless of theory, concepts or evidence! It was during my PhD studies when I focused on how patient-autonomy was experienced by older people in hospital that I began to focus on the ‘authenticity of persons’ (McCormack 2001). Coming to know how authenticity is central to who we are as persons provided a rationale for why so many nurses struggle with ‘applying’ pre-determined theories to patient experience. I conducted research that analysed 14 case studies of nurse–patient relationships. I developed a conceptual framework for person-centred practice based on an understanding of autonomy as ‘authentic consciousness’ (McCormack, 2003).
The Person-centred Practice Framework
The framework of authentic consciousness formed one of the core theoretical perspectives underpinning the current ‘Person-centred Practice’ Framework of McCormack and McCance (2017; 2019) – Figure 1. The Person-centred Practice Framework was derived from McCormack’s conceptual framework (2001, 2003) focusing on person-centred practice with older people, and the framework of McCance et al. (2001) focusing on patients and nurses experience of caring in nursing. The Person-centred Practice Framework has been adopted globally as a way of conceptualising nursing policy, practice, education and research. It has been used to inform care-delivery models (McCormack et al 2012), curriculum frameworks (McCormack & Dewing 2019), research methodologies and research practices (McCormack et al 2017). The framework sets out what we have determined, through more than 20 years of research and practice development, to be the key components of person-centred practice.
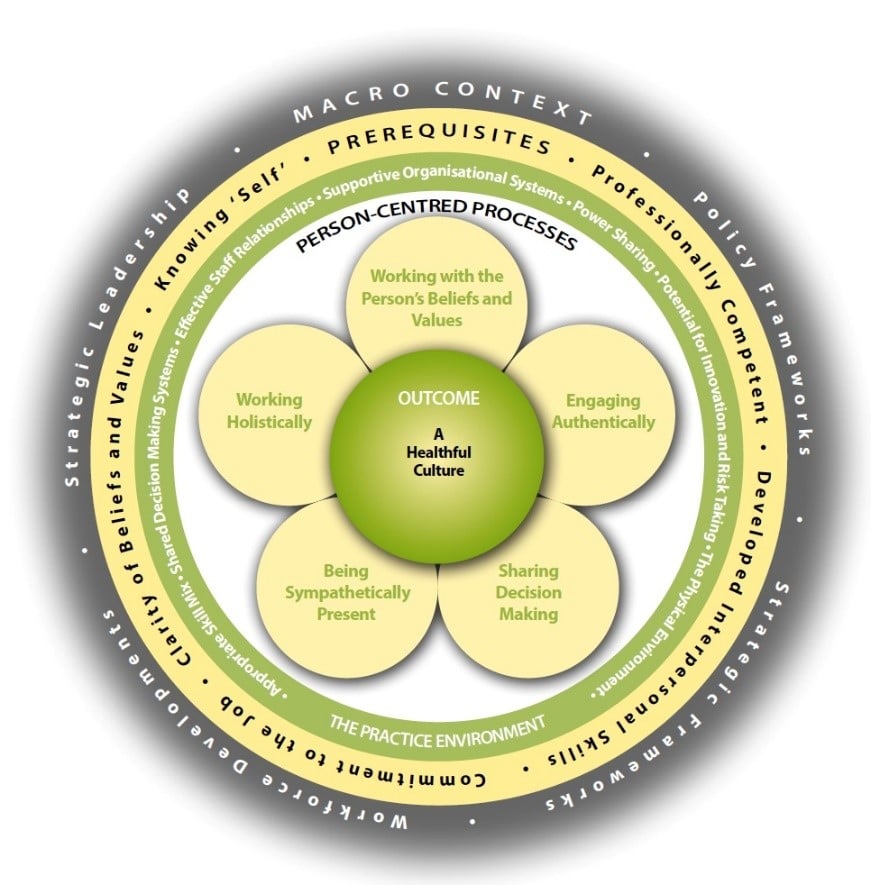
The Person-centred Practice Framework reflects the essence of human caring. Caring is a central concept in all health and social care practice, no matter the context or profession. Meaningful caring involves the interaction between values, beliefs and attitudes and is a far more complex activity than is often perceived, requiring intentional actions by health and social care workers. Caring requires us to know ourselves and in developing this self-knowing, care practices (such as washing, dressing, helping with food and drink, help with using the toilet etc) can be elevated from a series of tasks to opportunities for engaging with the whole person and with everything that is important to them in their lives. We define person-centred practice as:
“… focusing on the formation and fostering of healthful relationships with service users and others significant to them in their lives, as well as between all home care providers. It is underpinned by values of respect for persons (personhood), individual right to self-determination, mutual respect and understanding. It is enabled by cultures of empowerment that foster continuous approaches to practice development” (McCormack & McCance, 2017)
The definition of person-centredness by McCormack and McCance surfaces four attributes of persons and person-centred relationships:
- Respect for all persons
- Engagement and collaboration
- Individual and collective right to determine their own destiny
- Equity and equality
